Sometimes we consider workflow in the context of electronic health record (EHR) usability. We imagine workflow is a series of steps that are performed, usually in sequence, but sometimes with some variation in the sequence of steps. It's far more complicated. Holman et al [JAMIA 2015 Sep] recently published a report analyzing a large number of primary care physician workflows to conclude:
PCP workflows were unpredictable during face-to-face patient visits. Workflow emerges as the result of a “dance” between physician and patient as their separate agendas are addressed, a side effect of patient-centered practice.
Some workflows can be fairly simple. For instance, e-prescribing refills of a single medication (generic oral contraceptive) for a woman returning for her annual well woman exam. She has the same job, the same insurance plan, the same copay amounts, and the same medication. These details make this particular e-prescribing workflow simple. This can be done with fast, recognition-based, System 1 thinking which takes little cognitive effort. [Kahneman, Thinking, Fast and Slow].
Now by contrast, imagine an older patient with 8 different medications and as many chronic problems. Some of the medications are more expensive, because they're not available generically. Thus there are more opportunities for dug-drug and for drug-disease interactions. There may be opportunities for dual benefits from a new prescription that benefits more than one problem. If the insurance plan has changed since last year, then copays and coverage may be significantly different and thus require the attention of the physician and patient. In some cases, prior authorizations may come into play. This process requires system 2 thinking, deliberative, slow and effortful, and requiring sustained attention.
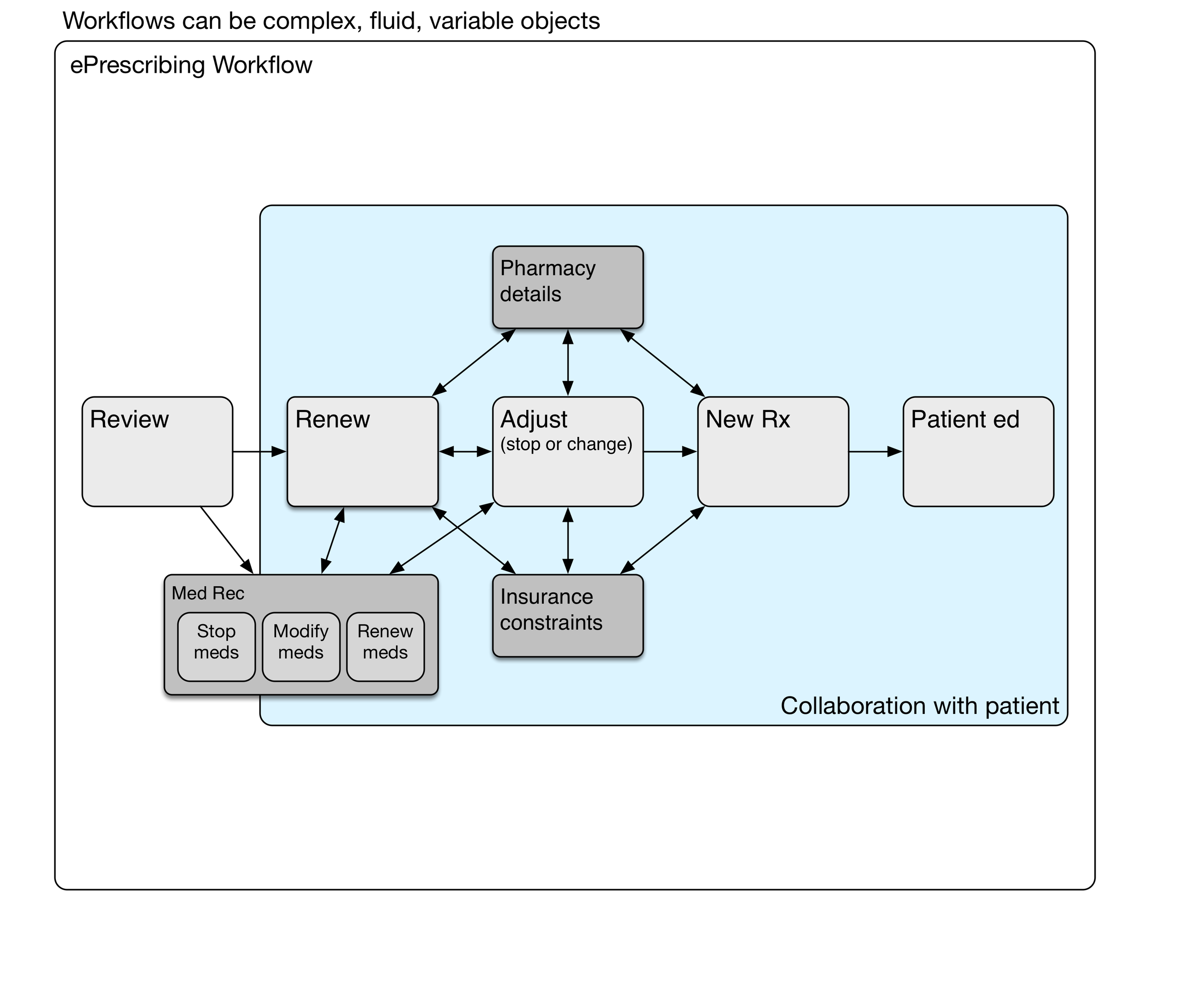
To appreciate the underlying complexity and mental effort, let's take a look at a simple e-prescribing workflow model, and then drill into the details.
e-Prescribing Workflow
Here's a diagram showing a simple e-prescribing workflow. The physician reviews the current medications and problems, takeing care of any renewals needed. Some of the medications may need adjustment, such as a change in the number of daily tablets, switching to a new drug strength, or stopping the medication. New medicationss may be prescribed. Finally, the physician and patient have a conversation about what to expect from the new medication. Written materials may be provided by the physician, although pharmacies provide those written materials more commonly.
Medication Reconciliation
Medication reconciliation may be done at the review stage, during medication renewal, or later adjusting medications.
We haven't mentioned medication reconciliation (med rec) yet. It may be a part of some ambulatory encounters, particularly after transitions of care such as hospitalization or emergency department visits where medication lists have been changed. When should med rec be done? Can it be done more than once during the encounter? Does it need to be done for every encounter? Medication reconciliation is a sidetrip in the e-prescribing workflow.
Renewing Medications
The timing of the next appointment determines which meds need to be renewed.
The decision to renew a particular medication depends on when the next anticipated visit would occur. Sometimes this is a matter of routine, such as every three or six months for someone with diabetes. That maybe once a year for somebody with high blood pressure. Fairly often, the interval is determined by newly identified clinical needs and negotiation between the patient and physician.
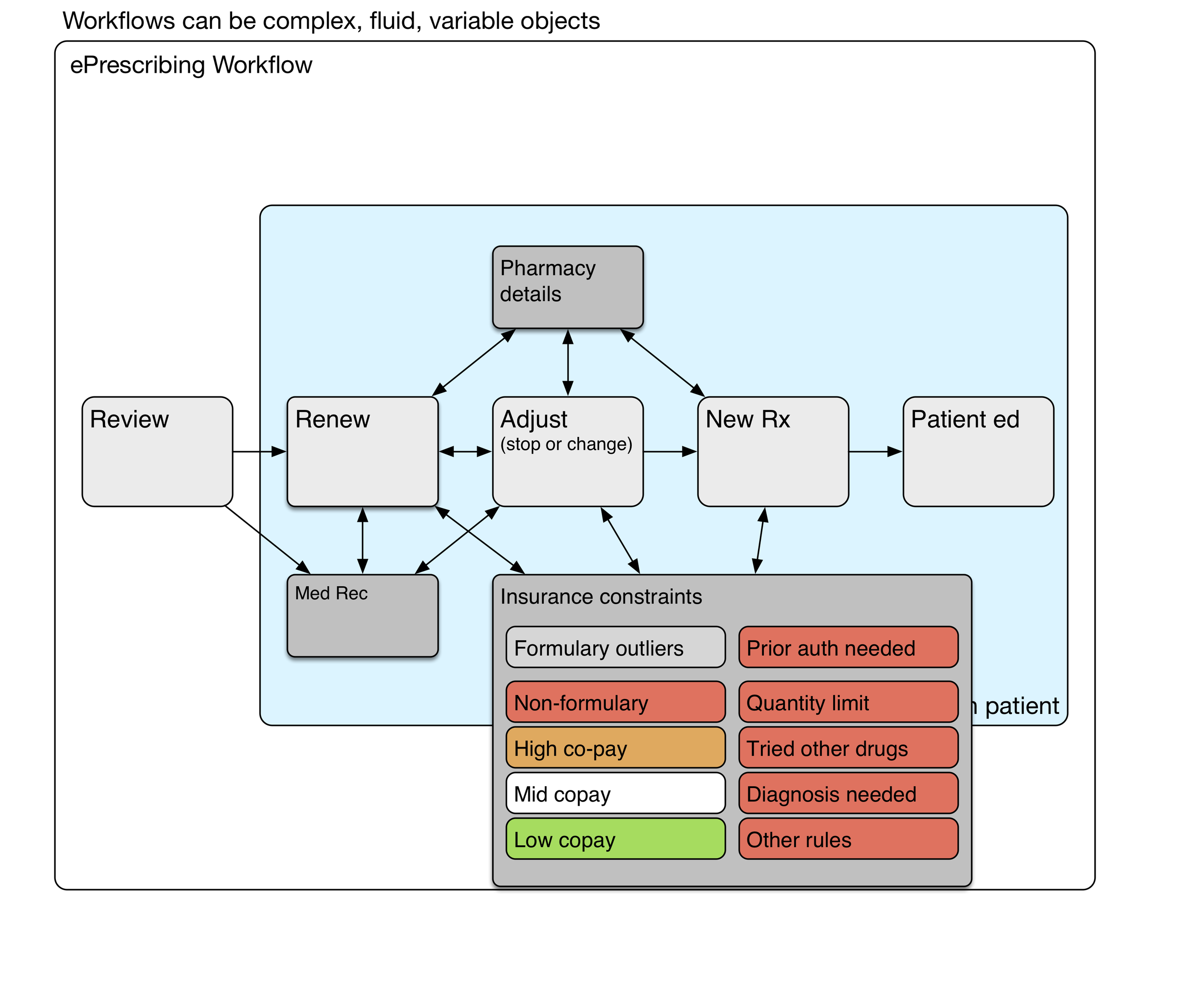
Pharmacy Details
Hotter colors (red, orange) depict greater cognitive load.
Sometimes it's simple. For an annual visit with no new medications and nothing changed, renewing all the medications may be as simple as a handful of clicks. However, if different prescriptions have different destinations (controlled substance prescriptions must be printed, some go to a mail order pharmacy for a 90 day supply, and others go to a local pharmacy for a 30 day supply), then it can get complicated. System 2 thinking again.
Insurance constraints
Hotter colors (red, orange) depict greater cognitive load.
Depending on the insurance formulary, some medications may have higher co-pays, and those copays can be unaffordable for many patients. Formulary visual cues at the point of care can lighten the physician's cognitive load somewhat. Nevertheless, it takes deliberate effort to find formulary alternatives that will be less expensive for the patient. The choice of an alternative medication is a collaborative process involving the patient.
Some medications (expensive, risky, or commonly overprescribed) require prior authorization by the insurance plan. This is a time-consuming process that will occur after the physician visit has been completed.
Workflow and subroutines
These subroutines are the deeper processes that are mentally effortful, variably performed, even sometimes avoided (due to time constraints or a physician's saturated mental capacity). The system 2 thinking it requires carries a heavy congnitive load. Remember that health IT workflows can be quite variable and complex